Education
Our program has a dedicated 60-minute daily morning report and lecture that is attended by all residents.
Occurring most weekdays from 0745-0850, the first 20 minutes is Morning Report which reviews recent admissions and highlights a case presented by an intern or junior trainee. Morning Report is led by the senior pediatric resident. This role for a senior resident is unique among pediatric residencies, and is aligned with the reality that our graduates practice as the local pediatric expert in remote locations where they must teach and lead medical teams who may not have much pediatric experience.
A 40-minute lecture follows morning report. Lectures are approved for CME credit. Topics are aligned with the American Board of Pediatrics content specifications. The first month deals with emergency and acute care pediatric topics from all specialties including general outpatient pediatrics.
Various other topics covered during morning report:
- Clinicopathologic Cases
- CPCs are capstone teaching conferences presented by our PGY-3 residents. The resident guides the audience through a patient case, diagnostic decision-making process, differential diagnosis, and cost analysis. The presentation is performed in conjunction with a faculty advisor and field experts who highlight salient points from the case and perform pathologic specimen correlations.
- Journal Club
- Occurring monthly during morning report, interns are given the opportunity to critically analyze and present a pediatric-relevant research article with assistance from a chosen mentor.
- Morbidity & Mortality Cases
- Morbidity and Mortality Conferences are held as an opportunity to review and learn from experiences in healthcare that result in unintended patient outcomes: morbidities and mortalities. These conferences support a systematic review of patient complications of care and deaths in order to improve future patient care and professional learning. The conferences are intended to be blame free and encourage transparency.
Please see the academic calendar or the Plan of the Week for more information.
The Uniformed Services University of Health Sciences (USUHS) Pediatric Grand Rounds are designed to improve the broad practice of pediatric medicine, including patient care, healthcare research, medical education, public health, military medicine, and innovation.
The USUHS Department of Pediatrics and all School of Medicine faculty, National Capitol Consortium staff and trainees, Walter Reed National Military Medical Center staff, and military physicians throughout the world are welcome to attend this bimonthly lecture to learn about pediatric topics, research, and challenging clinical cases.
Time: The 1st and 3rd Wednesdays of the month @ 0745 Eastern Time
How to attend: Pediatric Grand Rounds is presented in person at either lecture hall A2 or A3 on USUHS medical school campus. It is also simultaneously broadcasted via Zoom.
Occurring every continuity clinic day from 1215-1300, faculty and residents discuss common pediatric topics and conditions.
The NCC Pediatrics Residency and the Department of Pediatrics are leaders in Quality Improvement and Patient Safety initiatives in Military Medicine. Our faculty were Principal Investigators and our program was a test site for the I-PASS Handoff Study that is now the standard at Walter Reed Bethesda and military & civilian hospitals throughout the country and world. The Department of Pediatrics also brought the concept and practice of patient-centered (rather than location-centered) safety huddles to Walter Reed Bethesda. Residents and faculty routinely participate in the weekly Safety Huddle and systematically review all patient safety reports that involve children - no matter where in the hospital they occur.
Resident Quality Improvement Curriculum
All residents train in Quality & Patient Safety through the Institute for Healthcare Improvement. Residents form & join teams comprised of residents, faculty, medics, nurses, and administrative personnel toconduct performance improvement project each year. Projects are aligned with the American Board of Pediatrics Maintenance of Certification (MOC) Program for Earning Part 4 MOC Credit. Residents can receive Part 4 MOC credit that is 'banked' for their first 4 year cycle after residency graduation. Meaningful participation in a NCQA-certified Patient Centered Medical Home also earns Part 4 MOC credit. Faculty and residents submit their proposals, projects, and PCMH participation through the Maintenance of Certification Activity Manager
PI/QI Projects
The NCC Pediatrics Residency has a strong active research community in pediatric basic science, clinical studies, and educational research . Primers on conducting pediatric research are incorporated into the morning lecture series. A constantly updated online database of projects and mentors is available. There are many active protocols initiated by our residents. The Scholarly Oversight Committee for Residents (SOCR) was created to track resident Advocacy-Research-Military (ARM) projects and help facilitate resident scholarly activity. The committee is composed of faculty and fellows who have research and mentorship experience and can offer guidance on scholarly work.
Occurring every month, all residents are able to join for an afternoon of dedicated education led by one of the subspecialist teams. Most academic half-days involve hands-on and group activities. The afternoon typically ends after a housestaff meeting.
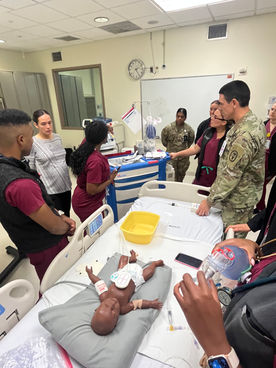
Occurring once to twice a month from 0745 to 0850, residents are given the opportunity to simulate important procedural skills (e.g. central lines, chest tubes). All interns become qualified in PALS, NRP, STABLE as well as ACLS and ATLS. Residents are required to become NRP, STABLE, and PALS instructors by the time of graduation. Residents also take the Pediatric Fundamentals of Critical Care Skills Course (PFCCS) and Military Medical Humanitarian Assistance Course (MMHAC).